Cirrhosis
 MASH is a leading cause of liver
cirrhosis in the US2
MASH is a leading cause of liver
cirrhosis in the US2
-
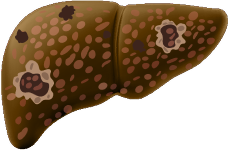
Cases of MASH with cirrhosis in adults are expected to increase ~2x from 2020 to 20503
-
22% of MASH patients with F3 progress to cirrhosis within 2 years4
-
Patients with cirrhosis (F4) have a 42x higher risk of liver-related mortality vs F05